
The following piece by DCIS Understood Founder Julia Stalder was published in CURE Today on June 17, 2025.
The bad news is you have ductal carcinoma in situ. The good news is that DCIS is the best type of breast cancer to get.
Those were the words of the pathologist delivering my biopsy results. I was holding the phone in one hand and packing a suitcase with the other. It was February 2024, just days after my father-in-law had passed away, and I was preparing my family to travel from New York to Pennsylvania for his funeral. Emotionally overwhelmed, I had no space left for new trauma—so when I heard “DCIS (ductal carcinoma in situ),” I hoped it might be another benign blip on the radar of my dense breasts.
I had never heard of DCIS. “So, what are the next steps?” I asked, channeling my inner Type A. The pathologist replied, “You need to schedule an appointment with a breast surgeon.” When I asked if it could wait, he gently urged me to get started.
I was 43. And DCIS it turns out, is very real.
Understanding DCIS and Treatment Challenges
A few weeks and tests later, I had my full diagnosis: two small areas of low- to medium-grade DCIS in my right breast. The pathologist had been partly right— ductal carcinoma in situ is technically the “best” kind of breast cancer to get— but what he failed to mention is that DCIS is the hardest to know how to treat.
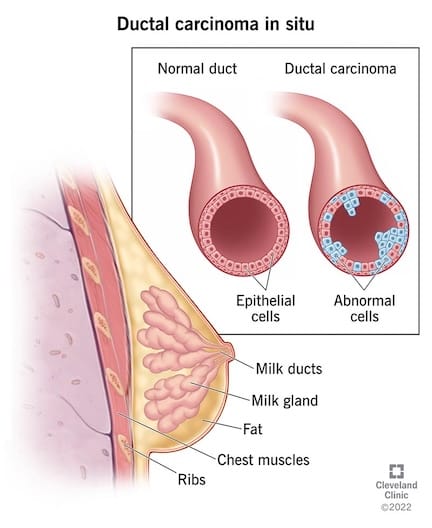
DCIS, often referred to as “stage 0” breast cancer, is a pre-invasive condition where abnormal cells are confined to the milk ducts and have not spread to other parts of the breast or body. It can, but often does not, lead to invasive breast cancer. Studies estimate that 50–80% of untreated DCIS would never become life-threatening. Yet, because we can’t predict which cases will progress, nearly all are treated aggressively: surgery, often followed by radiation and five years of hormone therapy.
The lack of certainty and consistency around DCIS that I encountered was staggering. Each of the three breast surgeons I consulted with explained it differently. Even the terminology varied—ranging from “a precancerous condition” to “cancer just lying in wait.” I was anxious and confused. I fell down the DCIS information rabbit hole, and the questions abounded: Was this cancer? What was my real risk of invasive disease? Why is there so much uncertainty surrounding a condition that accounts for nearly a quarter of all breast cancer diagnoses?
Ultimately, I learned that the science simply isn’t there yet. We can estimate risk based on certain factors, but there’s no definitive way to know if or when DCIS will become invasive. More research is urgently needed so that doctors can provide personalized care and avoid both under- and over-treatment.
Redefining DCIS Treatment: How I Found Confidence in Active Monitoring
As I began to understand more about DCIS and the emerging research, I felt increasingly uncomfortable with the idea of undergoing a mastectomy (the surgical recommendation) for a non-invasive condition that might never threaten my life. During my research, I discovered clinical trials in the U.S. and abroad exploring active monitoring as an alternative to immediate surgery for low-risk DCIS. Active monitoring—a long-accepted management strategy for some prostate cancers—involves closely watching the DCIS through imaging and exams, with treatment only if and when there are signs of progression.
My first two surgeons dismissed the idea, citing a lack of data. But at my third consult, I met a surgeon who was an investigator in the U.S.-based COMET (Comparing an Operation to Monitoring, with or without Endocrine Therapy) trial and had access to early results. He told me outcomes looked promising for patients like me. Although the trial was closed to new participants, he was willing to follow me under an active monitoring plan.
I said yes.
I currently alternate mammograms and MRIs every six months, take a low-dose of Tamoxifen, and live my healthiest life. So far, my DCIS has remained stable. I sleep well at night, knowing I can change my mind and have surgery at any time. In December 2024, the publication of the first COMET results confirmed what I had already come to trust—that active monitoring is a safe and reasonable option for certain patients, at least in the short term.
Beyond My Personal Journey: Starting a Movement for DCIS Awareness
After making my treatment decision, I felt a sense of peace about my health. But I couldn’t shake the feeling that too many women were facing this same confusing diagnosis without access to clear and up-to-date information. I was lucky to have the time, support, and resources to research my options. Most patients don’t. And when they turn to online resources, DCIS is listed as one of many “types” of breast cancer, with little information about the nuance surrounding the condition, let alone the latest research. That only fuels fear—which leads to knee-jerk decision-making and overtreatment.
That’s why I founded DCIS Understood, a nonprofit organization dedicated to educating and supporting DCIS patients. We offer clear, accessible information about the condition, treatment options, and emerging research, empowering patients to make individualized, informed decisions.
DCIS deserves its own advocacy movement. My goal is to ensure that women facing a DCIS diagnosis have a place they can turn to for trusted information and support in making the treatment decision that feels right for them.
Because when patients better understand DCIS, they can choose a path forward with confidence. I know I did.
Because No One Should Navigate DCIS Alone
Subscribe below for the latest DCIS news and updates.